Inflammatory Bowel Disease (IBD) – A Personal Perspective in Orthopedics
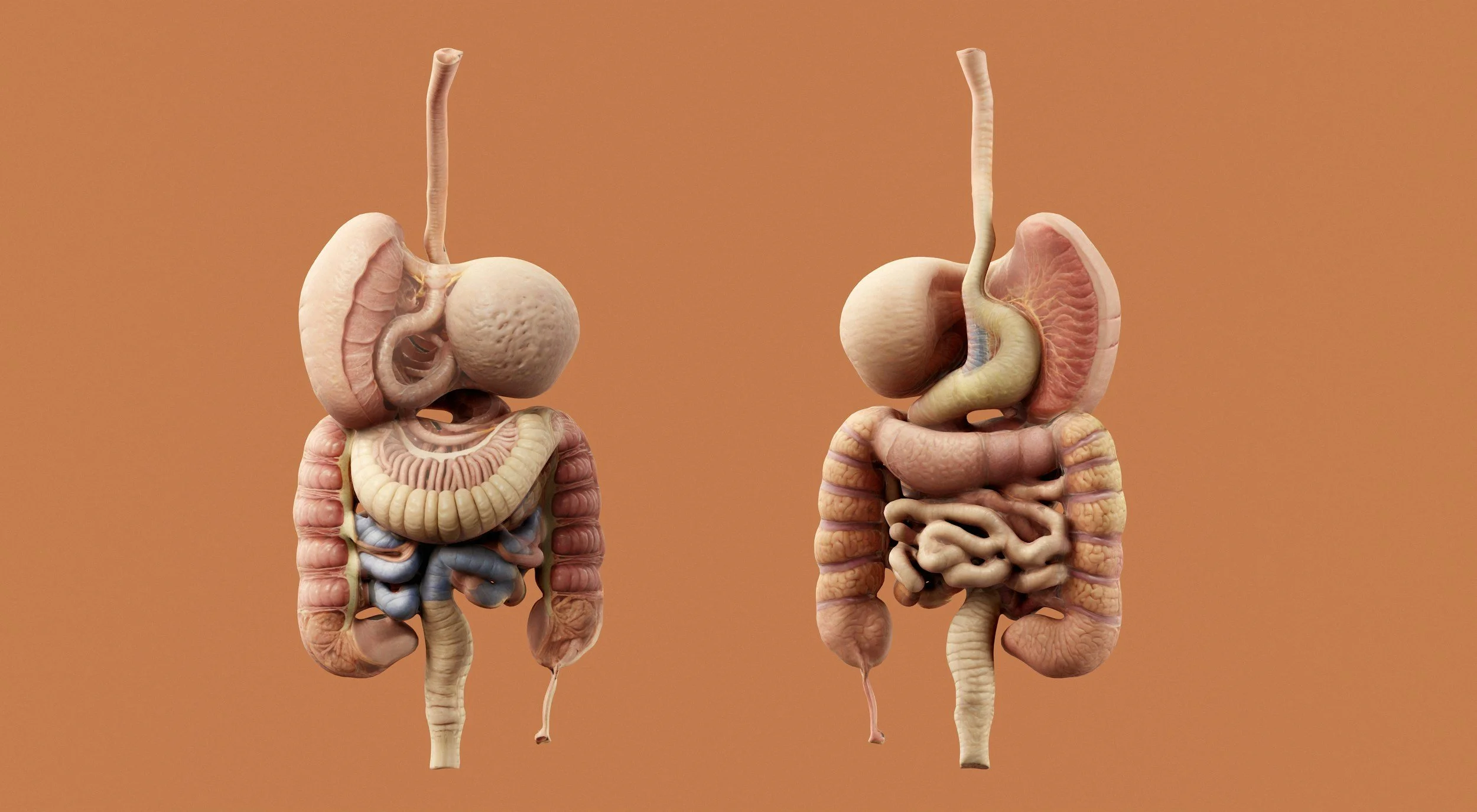
Inflammatory Bowel Disease is often thought of as a gastrointestinal condition — Crohn’s disease, ulcerative colitis, abdominal pain, flares, medication adjustments.
This part of my practice is deeply personal.
I have Crohn’s disease.
My father has ulcerative colitis.
I grew up in and out of Children’s Hospital of Philadelphia, and I spent five years on human growth hormone therapy as a kid. Those experiences — being a patient first — are what led me into medicine. They shaped how I think, how I communicate, and how I treat the people sitting in front of me.
For many people, IBD reaches far beyond the gut. It affects energy levels, joints, tendons, the immune system, mood, and daily life.
How IBD Shows Up Outside the Gut
Many patients with Crohn’s and ulcerative colitis experience extra-intestinal symptoms, including:
Joint pain or swelling (arthritis associated with IBD)
Tendon and enthesis irritation (enthesitis)
Back pain or sacroiliac joint inflammation
Persistent fatigue
Side effects or reactions to biologic medications
These symptoms can easily be mistaken for:
“Normal orthopedic issues”
Overuse injuries
Age-related wear and tear
Or, sometimes, dismissed entirely
That’s where things get complicated — and where thoughtful evaluation matters.
Where Orthopedics and Gastroenterology Meet
My role is to help answer an important question:
Is your pain coming from the musculoskeletal system itself, from your immune system, or from your medication?
I work closely with gastroenterologists and, when needed, rheumatologists to determine:
What is inflammatory vs. mechanical
What requires medication adjustment vs. physical therapy vs. procedure
How to treat the issue without disrupting IBD control
There is rarely a single “right answer.”
But there is a right approach:
Slow down, listen, examine, think, collaborate.
Why This Matters to Me
I’ve sat in the chair on the other side of the exam room.
The uncertainty.
The back and forth between specialists.
The sense that no one is looking at the whole picture.
I’ve seen IBD patients bounce between:
GI
Primary care
Orthopedics
Rheumatology
Trying to figure out what’s driving their symptoms.
So I try to bridge the gap.
I take the time to understand what your body has been through — the medications, the flares, the surgeries, the setbacks. I look at the clinical picture through a lens that includes both the musculoskeletal system and the autoimmune story behind it.
My Goal
To help you move, perform, live, and feel like yourself again — without dismissing the complexity of your condition.
For me, it’s not just clinical.
It’s personal.